In this week’s interview, Chief Correspondent Steve Scher talks with Dr. Nathan Price of the Institute for Systems Biology. They outline the science behind systems biology, exploring it as an attempt to quantify the components that make up a biological system and then work together in concert to achieve life. Price delves into “P4” medication—medicine that is predictive, preventive, personalized, and participatory—as a way to encourage wellness and prevent disease before it starts. Price speaks to genomics as a key to understanding our health, and highlights the possibility of expanding and redefining human senses. Get an insider’s look and stay in the know about what’s going on in this moment at Town Hall Seattle.
Episode Transcript
This transcription was performed automatically by a computer. Please excuse typos and inaccurate information. If you’re interested in helping us transcribe events and podcasts, email communications@townhallseattle.org.
Welcome to in the moment a town hall Seattle podcast where we get you excited about people coming to our stages by getting you familiar with our topic, personality and interests. I’m your host, Ginny Palmer. Caring for the health of the individual may be helped by discovering biological patterns in sets of big data, our genome or DNA, the cells in our body and the skin we slough off. These all contain vital information about our bodies that we could provide healthcare professionals and this information can help guide individual therapies and treating our individual conditions from disease to blindness to how the brain creates new pathways to move paralyzed limbs and prosthetics. The Institute for systems biology is at the nexus of individual health and big data in 20 years since its inception by dr Leroy hood and a team of scientists, ISB has been studying ways to integrate biological data from individuals so as to explore global dynamics and discover useful patterns.
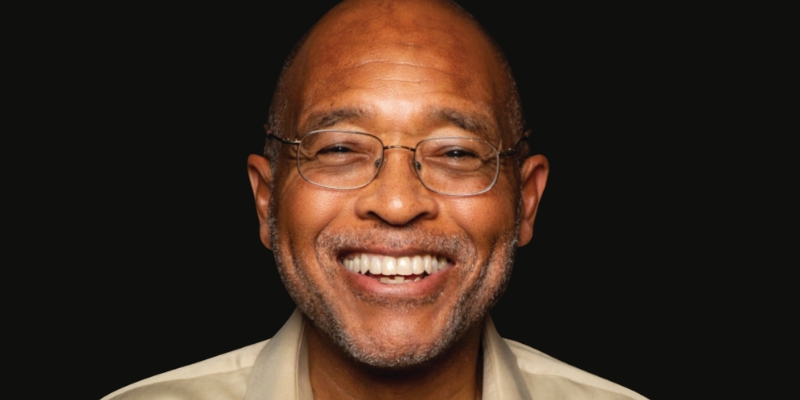
Dr. Nathan Price is professor and associate director of the Institute for systems biology. He co-directs the hood price integrated lab for systems biomedicine. He’s also affiliate faculty at the university of Washington and the departments of bioengineering, computer science and engineering and molecular and cellular biology. On March 5th Dr. Price will be moderating a panel at town hall in honor of the institutes 20th anniversary. The question before the panel will be, can we create new senses for humans and will feature Dr. David Eagleman who studies sensory substitution, brain plasticity and synesthesia. Together they will explore a new knowledge about the brain and innovations and seeing patterns through biological data that can bring about better individual outcomes. They will also talk about Eagleman his new book Livewired the inside story of the ever-changing brain. Our chief correspondent, Steve Cher, sat down with Nathan Price at his office in Seattle’s South Lake union neighborhood to talk about big data biology and human health.
Thank you for talking to me first of all, I appreciate that. My pleasure. Happy to be here and I like your office. We’re in your offices. Let’s see. Of all the things that stand out for me in this office of of the many cool things that are on the wall, pictures, posters is what I expect to see all over every new scientist office, which is just one wall that is a whiteboard. Are you always working on that? The whole wall is just painted so it’s all a whiteboard and so we could just brainstorm and come up with whatever we want to up there. So that’s fine. And, and I’m like are like there, there’s a of what is that a protein or something that’s going to be working as a protein? Is that the level you’re working at? Cellular. Biological.
It’s more, yeah, cellular, biological. In this case it’s looking at trying to build models of metabolites and proteins and construction that’s coming out of a, an organism. And one of the things we’re really excited about on the metabolic modeling is looking at pregnancy in particular because there you actually have to recreate an entire person. And so we’re, we’re launching this, it’s not the subject what we’re talking about today, but we are going to lodge next year, a huge project around this, uh, around, uh, pregnancy. Uh, but basically it is the biggest single, you know, perturbation that anyone goes through, you know, during a normal life and it grows in these spurts. And so you have to have these, uh, uh, kind of nutrient requirements that have to come together in order for you to do the next spurt and so forth. And so that, that drawing is, is kind of aimed at a, a model of that. But that’s a little off topic.
No, I like it. It’s just, it was so, cause one of the things I was struck by and doing a little reading and looking at work is you seem to have a lot of joy for this work. Is that fair to say? I know I’m ascribing something, but you seem to have that. Do you know why, where that comes from?
It’s a good question. It’s, uh, I find what we do every day to be fascinating and it is, uh, it’s the kind of job where you can, you can kind of dream about whatever you want to do and then you can go try to do it. You have to figure out how to raise the money forward. You have to get other people interested in it. You have to convince people in your lab that it’s a worthwhile endeavor. They don’t, I can’t just like dictate like, Hey, we’re doing this. Like they will tell me, you know, I’ve got to convince them it’s worthwhile.
Okay. Because in a sense, science doesn’t work that way. Dictation, you have to get people engaged.
Science doesn’t work that way because you, you need to have a passion for diving into problems because they’re very complicated. It’s very hard. And we could get into a long discussion on lots of reasons for that. And so you’ve got to love what you’re doing and you have to have a passion for it because if you don’t, there’s just no way that you’ll put in the hours and the time and the, the, you know, months and years of thought that and work and, and, and, uh, sticktuitiveness that it takes to like make progress on a problem. And so it can’t just be me. So whoever’s working with me on a team and we’re going to go on this problem, they have to be passionate about it too. So if they’re not passionate, it won’t actually happen either.
Yeah. You seem like you’d be fun to work with because you hold that passion. Do you hold that in your head? I’m going to try to be fun to work with.
I think I’m fun to work with. I’ve been told that sometimes not uniformly, you know, not everyone shares that opinion. Uh, you sometimes get the opposite, but uh, in general, uh, in general, yeah, it’s, it’s really a fun place. And you know, I co-run a research group here now with Lee hood who, you know, I know you’ve, you’ve met before who’s also got this of infectious spirit, which was partly what brought me here and what I was excited about. So I think ISB is a place where you can, yeah, you can dream big, you can be flexible. There’s not a lot of bureaucracy so you’re not, uh, you’re not blocked too terribly often from, you know, pursuing something. Reality may block you and does all the time, but you’re not artificially.
Let me touch on reality a little bit because you said science is hard. I’ve been spending a lot of time thinking about why we in this society today. Don’t think we’re in a fact based culture and sciences can, can remind us of that. That science is about the hard work. Even if it’s not perfect. You know, you think about climate change, Oh, it’s a, it’s a theory, right? But these are, these are people studying things and trying to come up based on hard data, hard numbers and hard and hard actual, you know, this means this, this means, this doesn’t mean this. Do you ever, um, I dunno, despair of living in a society where we’re not quite focusing on the fact that there are some basic truths.
Yeah. I think science is something that forces you to deal with, uh, with evidence in a serious way. And the culture of science. And it was interesting a couple of years ago I gave a, I gave a talk to a, let’s say a more broad kind of audience and I would say a sentence and all of a sudden people would cheer and you’d say another sentence, people would cheer. And it was so weird for me as a scientist because we never do that in science. Like the whole mindset of an audience at science. It’s not, Oh, I’m excited about what you’re saying. It is. Let me think about all the reasons why I do not believe what you’re telling me. You know, like you have to sort of prove it to the scientists. And I, and I love that about science and scientists and so it is frustrating I would say when we get into, you know, if you’re in discussions or if you’re in society and we say, Oh, you know, every opinion on this is valid and there’s, there’s a place of goodness that that comes from in the sense of inclusion and respect for other people.
And there is definitely a truth to truth is complicated and multifaceted. So there’s always different, different views, right? That can be very disparate, but from the standpoint of a scientist, certainly you have to at least agree on certain levels of evidence or the way that we’re going to, uh, accept or reject an argument. And that sort of just basic respect for, for truth, even though it’s complicated and can be seen from multi-facets, we still are trying to describe something that in, in some senses there’s a real, I think it’s really important.
Yeah. The concept of evidence as you, as you put it, is critical. Um, uh, all right. I want to read this sentence that you said and then I want you to unpack it a little bit. It’s just about what you do. Systems biology is beneficially transforming critical aspects of human wellbeing, including health, energy, and the environment, the science of systems biology, and the opportunity to drive it forward with such brilliant, engaging colleagues here at ISB excites me every day, which we talked about. But how about that first part, beneficially transforming critical aspects of human wellbeing, including health, energy in the environment. Um, let’s start with that. Help define that for me. What is this? What is the science of systems biology?
So systems biology is an attempt to first quantify all of the different components that make up a biological system and then understand how they work in concert to achieve a life basically. And so insists. So traditionally in biology for many, many years, the focus of a single person’s career could really dive in on a particular molecule, a particular phenomenon, because they’re so complicated. And we tried to store this wisdom about really tiny pieces of biology around, you know, sort of these scientific gurus who knew everything about it and had done decades of experiments and so forth. Uh, one of the real genius elements of, uh, you know, behind ISP. So, uh, founder, you know, Lee hood, who was one of the very early pioneers in this was to say, if we’re really gonna push out at scale and understand how these biological systems function, we have to get much broader than that.
And the beginnings of that are being able to measure a lot of pieces about biology. So Lee’s, you know, history, you know, here’s the founder of the Institute is famous in that he invented the automated DNA sequencer that made the human genome project possible. That was the first example, right? So we say, all right, we’re not going to study a gene, right? That used to be used to win a Nobel prize for figuring out the gene associated with a disease. Now we can, we can sequence the entire genome in a day for 1000 bucks or something like that right now. And you can do it a little cheaper at scale, but you know, look in that aside, but you can do it pretty easily. And now the notion of just being able to look at all that information, it’s kind of unthinkable. The first thing, at least in our minds, if you start studying any new organisms, the first thing you do is sequence its genome.
Cause if you don’t even have its genome, like what are we even talking about? Like you don’t have a map for anything. And so you can start doing that. And then you do the same thing with proteomics and Metabolon. You know all the proteins that you can measure, metabolites, all the small molecules and now you start having a sense for at least what is the component space in biology. Then you get into the really hard problem of systems biology is once you see all that information, how do you make sense of it? How do you put it together? And that’s what leads us more into trying to do the next step of that is network. So you’re looking at relationships between all of these different measures and on and on as you get up. So it gets very complicated in that sense.
So I told you, I went and pulled the, of a few of the papers that you’ve been a part of. And for example, one of them, a community driven global reconstruction of human metabolism. And then following that one is P four medicine has systems, medicine will transform the healthcare sector in society. Well those, those are examples of the kind of networking you’re talking about.
Yes. So those are, um, uh, pretty different examples. So I’ll start with the first one. So the first one, which we were a part of, uh, which was, uh, led by Bernard Paulson at, uh, UCS D along with an S T Lee, um, who is now out in Ireland. Uh, and burner Paulson was my thesis advisor when I was in grad school. So this was, you know, kind of a full circle coming back to some of the stuff I did 15 years ago. And so that study was bringing together an international consortium to build out the most comprehensive model we have today of metabolism in humans. So it pulls in together, you know, so you have thousands of reactions and metabolites and how they’re all interconnected. We’ve taken that subsequently and developed algorithms so that we’ve built models for 126 different tissues and cell types in the human body, uh, what they metabolize and so forth.
That’s the Genesis. That’s the basis by the way, of what we’re going to do in the project. I mentioned the very beginning with pregnancy is to use that as a, as a means to try to understand the metabolic demands placed on a woman as she’s going through pregnancy and uh, and how that relates to disease. So the second element there is P four medicine, right? And so P four medicine refers to medicine that is predictive, preventive, personalized and participatory. And so what we’re looking at there is trying to understand the signals, right? That are in all these complex networks so that we can predict disease before it starts prevention. We want to stop it so that it doesn’t, it doesn’t actually progress. This is a huge element. So Leah and I have initiated this field, we call scientific wellness, which is an essence. They try and understand from a quantitative state what wellness is or what, you know, how it, how it appears and what deviations from it look like so that we can intervene really early and stop a disease from progressing to where it becomes a, it’s really hard to, to treat.
And we could talk more about that. The personalized is, I think, self-explanatory every, it’s one of the real challenges in biology today with reproducibility and so forth is because every biological system is actually unique. Right? You and I are not exactly the same. We have, you know, we have our different life histories. Our genomes are very similar but somewhat but unique. And you know, there’s all those elements. And then participatory as a part of P four medicine means empowering individuals with information so that they can control their own health. And that’s another huge element that we’re really behind. And so those things come into play then, you know, and if we come, I keep bringing this up. You’ve got at the beginning of the, like the pregnancy study, as I mentioned, we’re doing all that with the metabolic networks, but it’s really to enable P four medicine because we see it as a situation where we can actually predict and prevent disease and prototype new approaches to that in a way that is, uh, that we can do quickly. And Alzheimer’s is another, you know, which we’ll get into is going to be, uh, another, uh, we’ll test another aspect of that.
So let’s, let’s talk about that specifically for a little bit. Cause aren’t you doing, uh, is it with the Providence, which is the, it’s Providence hospitals that you’re working with? Yes. And, and so how is that, how does, how does these quantitative ideas play out, you know, in a hospital? I know now we’re at the experimental stage, but how do they play out in a hospital setting?
Yeah, so this is an area that, uh, we’re really excited about. So a couple of years ago, ISB was, and for the first 18 years of our existence, we were a private, standalone nonprofit research Institute. Uh, and a couple of years ago, uh, Providence Saint Joseph health, uh, approached us and in particular, uh, Lee hood has become now the chief science officer for the Providence Saint Joseph health system. And ISB has become, uh, an affiliate of that system so that we are in part one of the research arms of, of Providence. Uh, we still, you know, mostly do independent research of various kinds, but, but we are, we have a mission as part of our mission now to, uh, translate into medicine. That was the big thing that brought our new president in. Uh, Jim Heath, why he moved up from Cal tech and came here. I was in part for that translational potential. So a lot of what we’re talking about, you know, certainly at the beginning was very theoretical and you’ve got to build out a lot behind it.
Uh, Lee and I became really interested in translating that out to society. Uh, we had, uh, about five years ago started a company called Arivale, which, uh, unfortunately now out of business. But, uh, what it did for about, uh, four years was to take individuals through a program where we generated for them, you know, genomics and a lot of clinical lab data and microbiome data. And, and we also did discovery work on proteomics and metabolomics and things of that nature. And it let us build up, uh, well it proved out a couple things. One was, uh, we were able to show that the data had a big impact on people’s health. Uh, and we have, um, you know, papers to that effect now. And it was a program that once people were doing it really made a difference. And the second was that by generating these data clouds, it was starting to give us all the information that you need in order to identify the early warning signs for the major human diseases so you can predict them and prevent them.
And that was the whole goal of what we were doing. We took about 5,000 people through that program. Now with Providence, uh, what we’re doing is with Providence Saint Joseph health, uh, is we’re going to be doing a pilot. Uh, we’ll, we’ll do 5,000 individuals in the coming year. But the big vision for that that’s being pushed forward, especially by Lee, is to get a million person, genome phenom project where we actually take and move into the clinic. What are the kinds of things that you can say that are actionable for people on their genomes? You know, a reason to do that, a reason that that matters are, and there’s a, there’s a lot in society happening on that front, coupled with the phenotype side because it’s really how the genome manifests, what’s happening in your environment, what’s happening in your lifestyle. And those things together we think will be totally transformative to health. And we’re, we’re pushing really hard with Providence to make that reality.
What do you mean by that? There’s a lot of things happening in society that can lead to that.
Oh, what I was alluding to is that genomics has hit a little bit of a wall recently. Uh, and it’s pretty fascinating. So, and I mean that from the commercial side. So a number of genomics companies, you know, have sort of arisen and, uh, have, uh, or fall in yellow certainly are, you know, ours was not ultimately successful. It wasn’t just genomics, but even 23 and me and ancestry, which are the most successful consumer genomics companies, uh, had major layoffs in the last a month. And what the phenomenon seems to happen at the moment is that genomics Rose, especially with those two pretty rapidly through your early adopters, the people that really wanted to know something about their genomics and they did that. And, but it has not yet translated to everybody wanting to do it. And there haven’t been as compelling of reasons for people to come back to it over and over again.
And we think those reasons actually exist. Health reasons. Yeah. Uh, but they, but you don’t actually get to them unless you do this next step of what we call, um, w under scientific wellness. But the manifestation of that genetic risk in the body, like what does it do and, and how, and what does it tell you that’s really meaningful. So genomics has pushed forward into the commercial space and into the community and had an had an impact. But the deliverables so far haven’t been of a quality that it has not yet convinced everybody out there that this is something that I need and that I need to go back to over and over again. So that’s what, why genomics has hit a little bit of a snack. I don’t think it is a permanent snack, but it is a huge, a challenge right now to then convey here are aspects that really matter about your genome, that that would motivate a, it’s incorporation. Now healthcare systems are starting to bring it in in a big way. Um, and that’s the other side of it.
Well, I mean one of the papers, a few of the papers that you were part of talk about big data. So is that how healthcare systems are bringing in and, and in other words, they can take some number of people and extrapolate some truths from that.
Yeah. Yeah. So I can give a, so healthcare systems are getting involved in this. There was a big partnership between Amgen and inner mountain, for example, where they’re now, which is a big healthcare system in Utah and they’re now recruiting 500,000 of their patients was a quarter of their, I think it’s a quarter of their system, uh, where they’re doing genomics. Uh, the genome has proven really important for the development of new therapies. Uh, it actually, uh, helps, uh, pharma companies and so forth with target identification or prioritization, uh, very strongly. Uh, so that’s, you know, that is one, uh, one big element a second, and I’ll just share this partly from our own work and partly from others that I, I think, you know, indicates some of the kinds of things that you can think about it having meaning. So one element that’s interesting is if you look at something like LDL or HDL cholesterol white, which everyone measures, it turns out that the level of, um, we’ll just take one of them at the moment.
Let’s say the level of LDL cholesterol is pretty pro. You could predict it pretty well from your genome. So knowing nothing about your lifestyle or anything else, just a genomics signature alone predicts it pretty well. Now, what we did in a study, which was really fascinating, so this was people that were going through the Arivale program. And what we saw was that if your genome predicted that you would have high LDL cholesterol, Oh, I’m sorry, let me, let me back up briefly right now, right? There’s 2 billion in these blood tests, not just this one, but you know, broadly, uh, run across, uh, the healthcare system, United States, and we treat them all basically the same, right? So we say, here you are, here’s our, our, you know, normal distribution across the population. And you’re either high or you’re low. And that’s kind of what there is.
So with LDL, that’s what we do. We take people that have the same level of cholesterol right there, they have high cholesterol, and at the moment we don’t use anything about genomics. So if you have 150 LDL, then you have 150. All the alums just treated the same. So what we saw in our study is if we took people that had exactly the same LDL level, but we looked at people who are there because their genome predicted they’d be there, or people were who were there when their genome predicted that in fact they’d be much lower. It turned out that by lifestyle intervention, the people whose genome predicted they would be high, we saw no statistically significant difference in them being able to lower their LDL cholesterol by going through this wellness program for the top 40%. However, for the bottom 40% for the ones that were predicted that they, their genomes predicted they could go low.
We saw very significant reductions in the amount of LDL cholesterol that they, you know, the amount they were able to reduce it. So what that showed us, and it was the same for HDL, and so what that showed us was that you could predict the outcome of a lifestyle intervention from the genome. And so you could tell people in advance, you know, and you know, this is the kind of thing that will likely work for you. So one of the things that we’re going to be developing, which I’m very excited about, is we can then take everyone’s genetic prediction for all of these blood marchers. And we can say, here are the five or 10 or you know, whatever the right number is that you should be able to modify pretty easily in the following ways with last night eventually because your genome is going to be working with you rather than against you.
If you don’t have your genome, you can’t do any of that. You’re totally blind to that. Uh, and so we just think there’s a ton of that kind of thing. And then once it gets integrated into healthcare and you can see, Oh, actually makes a difference to you, you know, it makes a difference in how you feel it makes a difference in, uh, in your weight. You know, we’ve, we’ve seen some other really interesting signals for BMI and so forth like that we think we’ll have, we’ll have an effect. It gives people a reason to believe or reason to care how, how will that make healthcare? Um, sounds like I can see how it makes healthcare more efficient. How does it make healthcare also less expensive? So for one, consider the, the number of individuals, let’s just stay with LDL, HDL, the number of people who are on Statens.
Right. So, uh, there’s a, there’s a lot of over-prescription and I don’t want to get, you know, I’m not a doctor, I don’t want to get into the specifics of any particular case on this. But Nick Shork at, um, uh, down in San Diego who was actually by coincidence, Terry yesterday, but he, uh, he had a paper in nature where they went through and, and just reported on the number of people who benefit from taking the top 10 selling drugs in the United States and the top 10 selling drugs in the United States. One out of either the best of them, one out of four people that take it benefit and the worst one out of 25 people who take advantage of it. Right. So that’s big. So let’s take Statens. So if you could, if you could take a number of individuals and say, look, you’re the kind of person who could reduce, you know, this, uh, using lifestyle intervention more successfully than, you know, maybe we could get some of the people, you know, not on the Staton.
Right. And people can argue, you know, some people argue that everyone should take a stat and or whatever and you know, we can leave those debates. But as an example, you know, that’s the kind of thing that you could do. And all these drugs, by the way, they always, you know, they, you know, there’s benefit to them or we wouldn’t do them, but they also have downsides to them. People on Statens there’s a 9% increase in incidents of diabetes. So one of the other things that I recommend for, you know, just from a personalization standpoint or that I would sort of look at for myself is, you know, you go on one of these things, well I’d probably measure your, you know, the diet, the various diabetes markers that are out there, your hemoglobin a one C your fasting glucose, you know, your home IRR, that kind of stuff to see if that is triggering. Cause that’s it’s just known from epidemiology and in our studies when we looked at people on stats and not, yeah, we saw an elevation in a subset of people on those markers and then zone.
Does the science allow you at some point then to actually by looking at their genomes know which of those people may be susceptible to when taking sentence get that’d be susceptible to diabetes?
Yeah, I think that’s a real interesting question. We can’t say, you know, maybe someone out there knows it and I haven’t seen it, but I, I’m not aware of an ability to predict that yet from genomics. But you can definitely see the movement that direction from the blood markers. That I think is is pretty straight forward. The genomic prediction and we do have a clinical trial that we’re running right now on using genomics for the interpretation of hemoglobin a one C for people who are pre-diabetic because at least in preliminary data, you know, we won’t know the answer to this really until you know, that’s why we did the trial. But I noticed in the data set that we had generated from Arivale that for people who had a high genetic predict a risk for high hemoglobin a one C that if we looked at people who had, you know, the same hemoglobin a one C where we might say they’re in the prediabetic range, that it was a lower fraction for individuals that converted into diabetes for those that were at the really high risk.
So in other words, if you were pushed there by genetics, it wasn’t, it didn’t look to be as big a deal as if you were at the same level but not push there by genetics. And there’s, and there’s pretty good mechanistic reason for that because you can have variants that mean that the, uh, the residents’ time of your red blood cells is a little bit longer. So, you know, so if my red blood cells last 120 days and years last 125 days, well your hemoglobin a one C would be naturally a little higher than mine because your cells have a little longer time to accumulate this, the sugar residues on them. And so you just adjust. You just adjust the measure for that. And there’s, there’s a million of these things I see, which is why you’re excited because you are working in data, but at the same time, at the cellular level on individuals. So you can, you can make the connections with, with, through the science.
Yeah. And that’s what was amazing to us as we started putting together these data clouds. And what was interesting was, you know, we had so much opposition to this at the beginning, you know, there were so many people including in the building, you know, that just really didn’t think we should go about doing this. And it was a waste of time and money to, you know, to generate, you know, this much density of data around individuals. And we have just found it to be unbelievably informative. And you know, it’s just one of the things that we, we push and we actually are, I’ve set up infrastructure here to add this as an add on to multiple clinical trials. Uh, because if you take, you know, if you have this sort of core set of data that you’re going to generate and you apply it on every clinical trial.
And we built an infrastructure here now so we can do the data reproducibly. There’s a whole infrastructure across the country and with lab Corp, you know, there’s bank blood samples that gets spiked in so that we can normalize all the things that are done in, you know, one part of the country at one month against another part of the country at another month that, you know, all those kinds of things. And you put it all together and all of a sudden you start having a system where you start learning from every trial and you, your data from your cancer trial is relevant to the data in your multiple sclerosis trial, which is relevant to the data in your, uh, Alzheimer’s trial, which is, you know, and so all of which we’ve got going right now. And so you can, you can take those. And it’s one of the things I’ve been arguing to a pharmacist when I go around and speak to pharma companies, which is, you know, the five most valuable companies in the world are data companies and pharma, in my mind, waste an incredible amount of data that would be so useful to the future of human health because they do not build basically exactly what we’ve built, which I wish they would do a and just say, you know, here is a set of measures that you can do that’s deep on every single trial and you integrate it into a system or you can do machine learning across it and you just start learning.
And then every single trial you just get exponentially more information about how the human body is interconnected, how it works. Uh, you get increased predictive ability. You know, what’s really unusual when you see it and on and on. So, well, I wouldn’t be, I’m going to shift topics to, to what you’re going to talk about at town hall, but I wouldn’t be doing my due diligence without asking. So are there concerns from some people about misuse of the data or a misapplication of information in a way that targets, you know, people unjustly? Is that some of the concerns you can see?
Yeah, you certainly run into those concerns. Uh, and there are examples, you know, there are, there are examples of, of misuse of this kind of data. I do want to say that they are very rare compared to the number of positive uses. I mean, the vast majority of what people want to do with these kinds of data is to, is to solve disease and, and so there are very careful safeguards that are put on for privacy. Uh, and there are, genomics has its own issues with that because the genome is ultimately, you know, the code of view. Uh, and so there, there are those issues like that. Uh, of course just visiting my office today, you will have left 30 million copies of your genome on the chair. And so, you know, in the far future, the far future, it is something we’re sort of shedding all the time, which we never had to care about before.
But, uh, it is, and that’s why I think laws in the future are going to have to be very focused around the use of these data. It’s going to be very hard, you know, to put the genie back in the bottle in the sense that you know, that we’re not going to have an ability to do genomic. And for the simple reason that I just mentioned, like it’s, you know, it’s ubiquitous out there and, and there are, you know, genome sequencers now that are small enough, you can carry them around in your front pocket. I had one in my pocket the other day. And you know, they’re not quite accurate enough yet, but they’re, they’re not these behemoth machines. They used to be let’s not all of them. And so you, you can actually, yeah, it’s like it’s people on the podcast can see my fingers, but it’s, you know, it’s like the length of, it’s like the length of your finger sort of smaller than a smartphone, smaller than a smaller phone, thicker.
But um, and so, uh, so you can do that kind of thing. So, so privacy issues are very important. Uh, how we use this data is really important. One of the things that, that, that strikes me often and I, and I think about a lot though, is we often get into these dichotomies or these, these situations where we have on one hand, this gets back to our evidence in like reality from earlier. We have on one hand a reality which is unless we integrate a lot of genomic information with a lot of health information, we will never learn how, why and how we are susceptible to so many of the chronic diseases that we are dying and suffering from now and we won’t actually ever be able to know how to solve them if we don’t do that. That’s just the physical reality because you just can’t understand the data at this scale if you don’t have a lot of observations of it.
On the other side is something that is not a reality but is created by us, which is can we do this in a way where we don’t hurt each other by bad laws and bad uses and bad actors and and all of this in terms of what we actually do with the data and just philosophically, and I think those are all really, really important issues. But philosophically I would like us to try to center ourselves around the things that in reality have to happen for us to achieve that, to try to solve that while minimizing the issues that we actually do control ourselves, which is how do we treat each other? How do we set up our social contracts? How do we set up laws and so forth.
All right, let me just, let me ask you this just because when I, when we were looking at the, when I was looking at the town hall descriptions, here’s this descriptions of what dr Eagleman is coming to talk about. And then you are going to be, you’re going to moderate this panel with him and with the Mary Kay Ross. And this was the question that, that was put on the, on the Townhall calendar. Can we create new senses for humans? Uh, the Eagleman delivers an exploration of sensory substitution, time perception, brain plasticity, synesthesia and neuro law. Unless this is a, a science fiction movie, right?
Well, what are we talking about here? Yeah. So first of all, we’re super excited to have dr Eagleman come in and keynote the, the event, uh, and, and super excited also to have, uh, Dr. Ross, uh, uh, who has a good partnership with us. So in terms of what, um, uh, what David’s going to talk about, you know, and I won’t, you know, still has thought of, he’s going to bring a lot of really cool new things, but this whole notion of sensory extension is really a fascinating one. So if you look at the world around you, if you look at everything that you’ve ever experienced, everything that you’ve ever experienced has happened in your brain, and your brain is actually blind to the outside world in a sense, right? All it gets are these signals that come in, right? And so if you take your eyes right, we see a tiny sliver of the spectrum of electromagnetic radiation that’s out there.
Uh, and as we look at that spectrum of, you know, what we have, what we have is light. There’s no reason that what we actually perceive. It’s not special in any particular way. It’s special to us because it’s our lived experience. Uh, but there’s no reason that you couldn’t actually augment or see more of that. And in fact, we take advantage of that in ways that our senses don’t perceive. And we turn it into what our senses can perceive, right? The internet radio, um, you know, all these signals, you know, the wifi that’s in this room, right? We don’t see it, we don’t perceive it. But as soon as, but we, we have, we have receptors, right? We have our phones. It does it. And it turns it into something that we can see in a light spectrum so it can get into our brain, right?
And so there’s this whole notion of reality like that. And some of what I imagined that a David Eagleman will share are around the notion that with people who are deaf with people who have had their limbs amputated, there are means now that are actually already happened, that you can connect devices into the brain. So these signals can go into the brain and it can come through any sense, right? You can turn it into an audio sense. You could turn it into a feel sense, but your brain gets these signals and it can figure out what to do with them. You know, I saw there was a really moving, uh, event at the NIH a few years ago, you know, and they had, you know, a guy there and he was, um, you know, he was without arms, you hadn’t had arms, you know, for a long, long time.
And so they put these prosthetic devices and he was able, you know, he would train with his thoughts to be able to reach out and hold the hand of his daughter for the first time ever. And I, I’m about to cry again. I was just, it was so beautiful, uh, to see that because it was, um, just the emotion in it. And it was, and again, his, he’s controlling it with his mind because his mind over time was able to learn, you know, how to, you know, how this device was measured. And so it, it responds to the electrical signals and it does this and you know, so there’s ways to think about, you know, I mean, he, you know, hailing the blind [inaudible] and healing the lame and like all that kind of stuff through science, which is a very remarkable. And so I’m sure David’s going to talk about a number of those kind of issues about how do we actually extend, you know, what our perceptions are.
You know, how does that relate back to what you’re doing here? I mean, you invite him in part because there’s some connections. Yes. So, so we’re very interested in it because David Eagleman is been, you know, he did this, uh, you know, his special on the brain and he has, uh, his neuroscientists. And what we’re doing here is we do a lot in this realm of scientific wellness and, um, and before medicine that we’ve talked about, one of the big areas we’re interested in is brain health. And, uh, you know, and you know, our lab, you know, probably about a third of the founding of the lab is on Alzheimer’s disease. We’re working on that a lot. And basically what we’re excited about is the notion of trying to move upstream in Alzheimer’s. And what I mean, you know, I mean early on and have an effect on what it can, what’s happening downstream.
So we, uh, dr Mary Kay Ross who’s coming, she started the brain, uh, health and research Institute here jointly with us in Seattle, moved up from Savannah, Georgia. And what we have there is you have, uh, uh, what we, what we’ve got so far in Alzheimer’s diseases were about, Oh, for 400 on clinical trials with drugs of having an effect. There are a few trials where an effect has been shown, one of which is the finger study and it’s not a drug, but it’s various lifestyle interventions and lifestyle interventions early on seemed to have an effect. In fact, I went to Genentech a while ago to give a talk at their, you know, their neuro, uh, neurological division. And I remember the head of it, you know, as I walked in and said, don’t, she says, well, drugs have never worked. Lifestyle interventions. I think I’ve ever worked at Alzheimer’s.
I’m like, Oh, I thought I was going to fight you on that. Okay, we’re on the, we’re on the same page. Um, you know, people still keep working on the drugs like we need them. But what we’re excited about with Mary Kay and others is that they have these patients that have gone through these, these very personalized, multimodal therapy programs. And, and what they see is that, you know, in, in some, you know, in some of the individuals seem to have a pretty strong, um, uh, benefit from going through these programs, but they’re highly, um, multi-modal. They’re highly personalized or not as reproducible. And so there hasn’t been as much like really hard, you know, kind of clinical trial style evidence behind them. And so we saw that as really an opportunity, uh, to do two things. So first is to take and get access to all the information from into patients who consent and the identified information to track progress along with what’s being done so that we can start to establish an evidence base behind this whole space to say, okay, when we take a thousand patients that go through this, all right, what fraction benefit, how much quantify it.
So we’re, we’re very interested in trying to understand that from people that come in with mild cognitive impairment. Uh, you know, do we see real effects? So that’s a big element. And the second thing we want to do is to add on this, these data clouds we talked about. So we get this really rich depth of information so that for any individuals that go through there where we see an unusually large effect or you know, someone that really responds to something, who is able to cause there, there are these dramatic stories of the, of some of these individuals who, you know, talk about, you know, they’re having, you know, lost really key aspects of their memory and getting it back. You know, and so they’re, you know, and so you hear these things and so you want to establish a scientific credibility behind it, understand, you know, to what frequency is that happening, quantify the degree to which you know, which that happens in any individuals and then have an ability to dive in in a deep molecular way and say, okay, when we see these, you know, sort of outlier events, which you know, people see sporadically, you know, here and there, can we learn something from those so that we can develop therapies that are in fact much more efficacious if they’re applied early enough.
And all timers I think is a PR and dementia, I should say Alzheimer’s and dementia, sometimes it’s a dementia that’s not Alzheimer’s. But once you’re really far down that path and your brain is degraded, you can imagine some scifi kind of things to try. But it’s pretty impossible today to think about how you put that back together. But if you can intervene early and understand the processes that are driving it and as the finger study showed that these are at least to some degree modifiable, can you in fact make a difference if you find people early enough and had come up with good strategies. So that’s what we’re trying to do.
That’s wild. That’s wild to see how data works to that. That’s very cool. Um, all right, last just sort of question. You already touched on it. You’re here, Seattle children’s, here you dub Mary Ross’s Institute, the Allen Institute. Um, is there some value in being in a neighborhood where all this physical, where all this is happening? I mean, in a world of data and you know, and, and people can talk to each other across the world. Is there some value being all clustered like this?
A huge value actually. Uh, there are, you know, the university of Washington is a fantastic [inaudible] research Institute. I was actually just there this morning because, you know, I got an invitation to go, you know, to meet with the white house science advisor who is here in town visiting UDaB. And they were kind enough to let us have a representative from ISP come. And so, you know, I did that, uh, this morning. So, uh, the Hutch, uh, which is one of the greatest cancer research institutes, uh, that there are, you know, that there is in the, in the world. Uh, and I, I’m on the board of advisors for the American cancer society here in the area. So we do a lot of, uh, events and, and, uh, outreach with the Hutch. Uh, they’ve actually been really important to, uh, you know, major, uh, cancer grant that we’ve been working on.
You know, getting some bank samples from them has been really important. Uh, the, uh, Seattle children’s of course, which, uh, we have worked with, uh, on pregnancy and they funded one of the people in my group, Alison Paquette, you know, has a grant, uh, you know, uh, with, uh, some of the people there, which has been a terrific Sage Bionetworks here in town is one of the great, uh, uh, aspects of centering, of, of uh, open data. And we have multiple things we do with Alara mangrove VT. The presidents are just fantastic. Uh, the Allen institutes, uh, are here, right? And that’s an incredible, uh, resource of knowledge in artificial intelligence and the brain and cell engineering. And so it’s, it’s really, it’s a huge advantage and that’s why we tell people, come to Seattle.
It’s fun. It’s wild to think of that though, that it’s, you know, knock knocking on doors. Being able to meet people on the street is as much the connection. The networking is, you know, the networking you’re doing with the data. That’s very cool. All right. I appreciate your time. Thank you. Right. Thank you.
You can join Dr. Nathan Price. David Eagleman and Mary Kay Ross, founder and CEO of the Seattle based brain health and research Institute for wide ranging discussion of human health and biological innovations on March 5th at 7:30 PM and town halls. Great hall. Thank you for listening to episode 56 of in the moment. Our theme music comes from the Seattle band, EBU and Seattle’s own bar Souk records. You can listen to our town hall produced programs and speakers on our arts and culture, civics and science series, podcasts. You can also watch a whole library of content on our YouTube channel. Just search Townhall Seattle and subscribe to support town hall. Become a member or see our calendar of events. Check out a website, a town hall, seattle.org next week or correspondent Tom teacher will talk with Justin feral about wealth concentration and the environment. Till then, thanks for joining us right here in the moment.